If you’ve ever been told that a vertebra in your spine has “slipped,” you may have felt alarmed. In reality, what that phrase means and what it does not mean can make a big difference in how you move forward. At 100+Living Health Centres in Kelowna, we help patients understand these changes — and importantly, we help you choose what to do next with confidence.
In this article we’ll cover:
-
What happens inside your spine when one vertebra “slips”
-
The terms you may hear: anterolisthesis, retrolisthesis, spondylolisthesis
-
Why it usually develops slowly, rather than from a sudden injury
-
How we diagnose and measure it at 100+Living
-
How non-surgical corrective care (including our advanced-certified CBP approach) can help
-
What you can do now to protect your spine, posture and long-term function
-
When surgery might be considered —and when it often isn’t
What a “Slipped Vertebra” Really Means
When the words “slipped vertebra” come up, it can sound like something dramatic — as though your spine has broken or collapsed. That’s rarely the case. What you’re usually looking at is a subtle shift of a vertebra out of its normal alignment with the one below it.
The medical term for this is spondylolisthesis — a condition where one vertebra moves relative to the one beneath it. NCBI+2Orthopedic Reviews+2
When the vertebra moves forward (toward the front of your body) it’s called anterolisthesis. When it moves backward it’s called retrolisthesis. Wikipedia+1
In plain language: one of your spinal “blocks” has shifted a bit — and that can affect how the blocks above and below behave, how the supporting discs and joints handle load, and how the nerves sit in the surrounding space.
But here’s the key: this kind of shift does not automatically mean you must have surgery. Far from it. In many cases, with good assessment and corrective care, you can restore better alignment and reduce pain or symptoms.
Why It Almost Never Happens Overnight
One of the most surprising things to patients is that this condition almost always develops gradually — not the result of one big fall or accident. Here’s what typically happens:
Poor posture + repetitive stress
When you’ve spent years sitting, bending forward, slumping, or doing repetitive movements, your spine’s supporting structures (ligaments, discs, facet joints, muscles) slowly get worn. The more time you spend with less-than-ideal posture, the more pressure accumulates in certain spinal segments.
Disc thinning, joint wear, ligament stretching
Over time, the discs between vertebrae can thin. The facet joints (which help guide movement between vertebrae) can wear down. The ligaments that stabilise the vertebrae can loosen. These changes reduce stability. Cleveland Clinic+2Orthopedic Reviews+2
When the supporting structures weaken, one vertebra may begin to shift slightly. That’s your “slip.”
Compensation in posture and movement
As the alignment shifts, your spine and body compensate. Your muscles tighten around the segment, your posture may change (for example your hips or spine angle), and your nervous system may adapt to protect the area. This causes further stress, sometimes pain, sometimes discomfort.
Because this process happens over months or years, most people don’t notice when the shift begins — only when symptoms (pain, stiffness, leg tingling) show up.
So when your doctor or chiropractor says you have a “slipped vertebra,” it typically means: a subtle shift has occurred. Not that your spine has snapped or collapsed. Understanding that helps reduce panic — and opens the door to real corrective work.
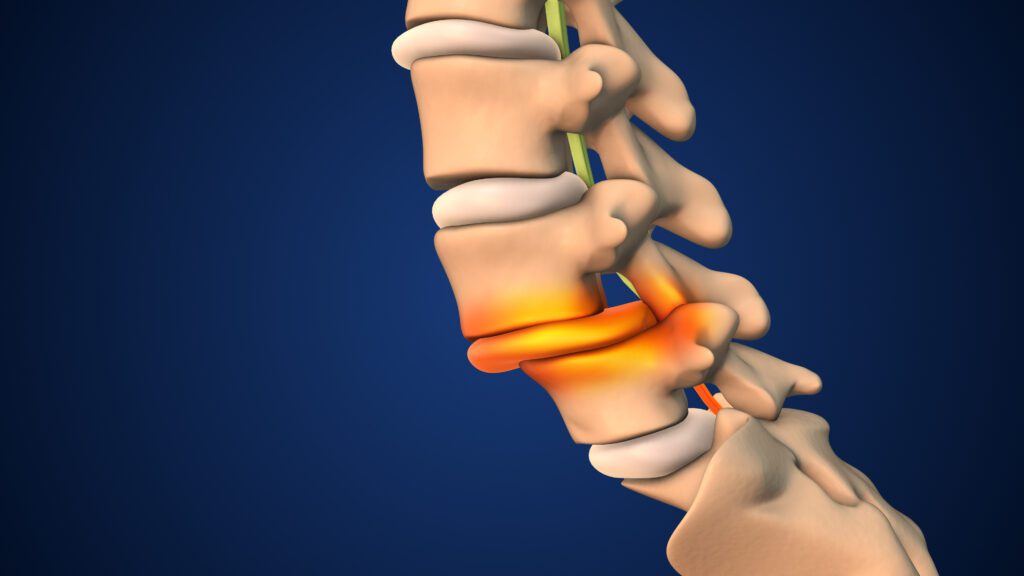
How the Slip Changes How Your Spine Works
Let’s visualise your spine like a stack of building blocks. Each vertebra sits on the one beneath it. When one shifts, even slightly, it can change how the whole stack functions.
-
The disc between the shifted vertebra and the one below becomes stressed in shear (sideways sliding) as well as compression.
-
The facet joints begin to take abnormal loads because the alignment is altered.
-
The ligaments that normally hold the vertebrae aligned begin to stretch or become lax.
-
The space for nerve roots may narrow, causing nerve irritation, leg pain or tingling.
-
Your muscles tighten and alter their activation patterns as they attempt to stabilise the segment.
-
Because the spine is one connected chain, other segments may adapt or compensate—so posture above or below may change.
A key point: having a “slip” does not mean your spine is collapsing. Many slips are mild, stable, and manageable. What matters is how far the vertebra has shifted, whether there is nerve pressure or instability, and whether you are experiencing symptoms. According to evidence-based literature, minor slips without symptoms often remain stable. BioMed Central+1
How We Diagnose and Measure Vertebral Slippage
At 100+Living, our goal is to assess the structural alignment of your spine precisely, so we know what we’re dealing with — then guide a treatment plan accordingly.
Imaging + posture
Many clinics rely on MRI or CT scans. These are helpful for seeing discs, nerves and soft tissue—but they are taken while you’re lying down, not standing. That means gravity and your normal posture are not considered. That can lead to missing how much the vertebra shifts during weight-bearing. Cleveland Clinic+1
That’s why we emphasise standing, weight-bearing X-rays. These show your spine under normal daily load. They allow us to measure how far one vertebra is off compared with the one below.
Grading the slip
We use standard grading systems (e.g., Meyerding classification) to determine how far the vertebra has slipped:
-
Grade 1: up to 25 % slip
-
Grade 2: 25-50 %
-
Grade 3: 50-75 %
-
Grade 4: 75-100 %
-
Grade 5 (spondyloptosis): over 100 % — very rare Physiopedia+1
-
Clinical practice shows that Grades 1-2 are mild to moderate and often respond to non-surgical care; Grades 3-4 require closer monitoring and may need surgical consultation. Cleveland Clinic+1
Instability matters
It’s also crucial to determine whether the segment is stable (i.e., the vertebra isn’t moving excessively when you flex/extend) or unstable (too much motion). Movement beyond ~3.5 mm in the lumbar spine is often used as a marker of instability (though each clinic may use slightly different thresholds). In general, instability increases the risk of ongoing damage and may steer treatment choices.
Putting this into your context
When you come in to 100+Living, we will:
-
Take a detailed history (how long you’ve had symptoms, posture habits, past minor injuries)
-
Assess your posture and movement (standing, sitting, walking)
-
Take weight-bearing spine X-rays and possibly other imaging if needed
-
Measure the shift, grade it, evaluate for nerve pressure and instability
-
With that data, we design your structural rehabilitation plan. (See our page on Structural Spine Rehabilitation for more detail).
Non-Surgical Corrective Care: Real, Measurable Results
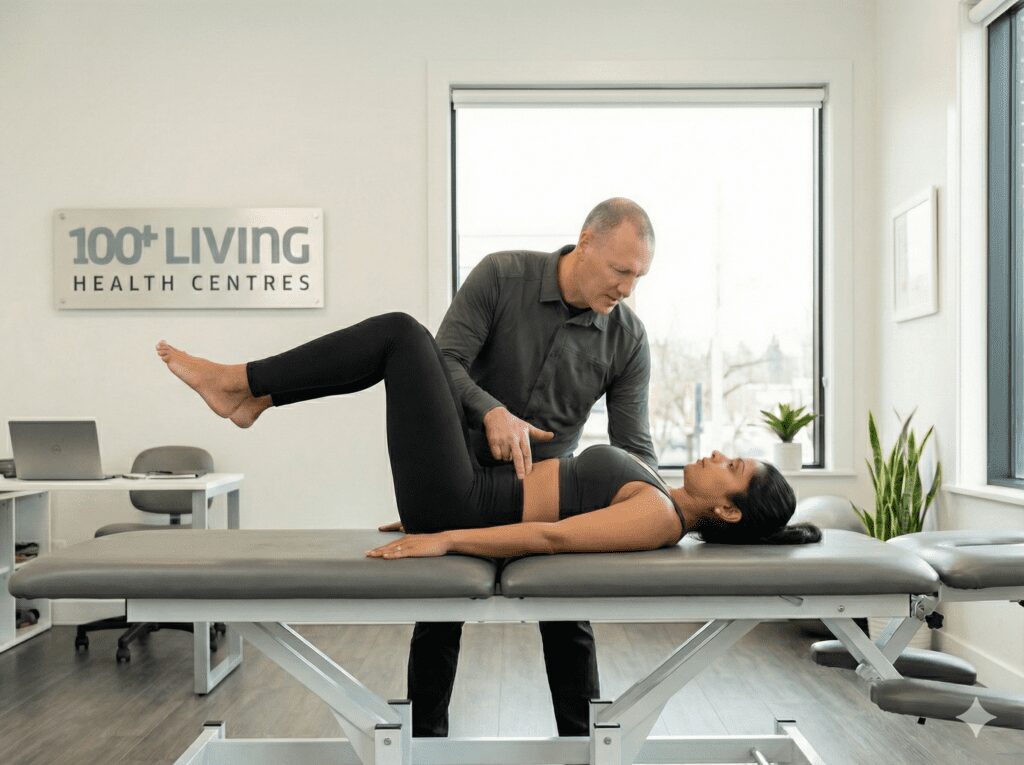
Here’s the good news: many mild to moderate slips can be improved with the right kind of care. At 100+Living Health Centres, we specialise in structural corrective care using the Chiropractic BioPhysics (CBP) method — a scientifically-grounded approach for posture and spine alignment.
Why our approach is different
-
We focus on correcting the cause (alignment, posture, stability) — not just managing pain.
-
We measure everything: alignment, shifts, posture, function — so we know exactly where you’re starting and track your progress.
-
We use advanced technology (such as our doctor-controlled traction system) and tailored exercise and adjustment protocols to improve structural alignment.
-
We combine posture correction, spinal adjustments, and targeted rehabilitation so your spine and nervous system learn to hold better alignment.
How the process works
-
Baseline assessment: standing X-rays, posture analysis, movement screening.
-
Individualised plan: based on your measurements, symptoms, grade of slip, posture pattern.
-
Corrective procedures: for example, specialised traction to guide the vertebra back into better alignment, posture-based mirror-image exercises, spinal adjustments.
-
Re-assessment & imaging: at set intervals we repeat posture/kinetic evaluation and X-rays to confirm structure is changing.
-
Maintenance & prevention: once alignment improves, we shift into stabilising exercises and posture habits to ensure long-term success.
What the research says
A “state of the art” review of lumbar spondylolisthesis (SPL) noted that conservative care has a place, especially for stable slips, and emphasised individualised programmes, education and graded supervised training. BioMed Central
The condition is common in middle-aged/older adults and gradual degenerative changes drive many cases — reinforcement that early structural intervention matters. The Spine Journal+1
In short: correction is possible, measurable and meaningful.
Why this matters for you
If you’re told you have a “slipped vertebra” (anterolisthesis or retrolisthesis), it does not mean you’re doomed or that surgery is inevitable. Many people achieve significant relief, improved posture, better function and long-term stability without ever needing a surgical option.
The key is catching it early, assessing it properly, and committing to structural rehabilitation.
What You Can Do Now to Protect Your Spine
While you’re waiting for your appointment (or between sessions), here are practical steps you can take to support your spine and posture.
1. Sit and stand tall
-
When sitting, keep your feet flat, knees at hip-level or slightly lower.
-
Use a chair with good lumbar support or add a small cushion behind your lower back.
-
Take regular breaks every 30–45 minutes: stand, walk, stretch lightly.
-
When standing, distribute your weight evenly. Avoid swaying your hips or leaning forward.
2. Move regularly
-
Walk, cycle, swim or other low-impact aerobic activity most days of the week.
-
Avoid long periods of static posture (sitting or standing without movement).
-
If your job involves repetitive bending, lifting or twisting — pause regularly and reset your posture.
3. Strengthen your core and glutes
-
Stronger muscles around the spine provide better support and help prevent further slippage.
-
Focus on: glute bridges, bird-dogs, planks, hip-hinge deadlifts with light weight and great form.
-
Consult your corrective care provider before starting heavy lifts or new regimens.
4. Use your corrective care plan actively
-
Commit to your plan: traction sessions, exercises, adjustments.
-
Track your progress: symptoms, posture, movement ability.
-
Be patient: structural correction takes time — but the payoff is real.
5. Monitor for warning signs
While many cases are stable, you should watch for:
-
Loss of bladder/bowel control
-
New, progressive weakness in your legs
-
Big change in walking ability or numbness spreading rapidly
If these occur, immediate specialist referral is indicated.
When Surgery Might Be Considered
Most mild-to-moderate slips (Grades 1-2) can be managed non-surgically. However, there are scenarios where surgery may be appropriate:
-
A high-grade slip (Grades 3-4) with instability causing nerve compression or progressive symptoms.
-
Severe neurological deficits (e.g., leg weakness or reflex loss, bladder/bowel problems).
-
Instability causing rapid worsening of the condition despite conservative care.
-
As the Cleveland Clinic notes: “Many people can manage symptoms… without surgery. But your provider will suggest surgical repair if the slip is high grade or non-surgical treatments don’t help.” Cleveland Clinic
-
Even in those cases, surgical involvement should ideally follow a clear assessment, weighing risks, benefits, and post-surgical rehabilitation.
Why 100+Living Health Centres Is the Corrective Care Choice
If you’re searching for a solution, 100+Living brings unique value:
-
Over 30 years of experience helping people restore mobility, posture and confidence.
-
One of the few clinics in Western Canada whose doctor is advanced certified in CBP (Chiropractic BioPhysics) — focused on true structural correction, not just pain relief.
-
We emphasise measurable change: standing X-rays, posture analysis, ongoing re-evaluations.
-
We use advanced equipment (such as our Robo-Trac traction system) to apply safe, targeted corrective forces.
-
Our goal: help you live strong, active and pain-free for as long as possible — not just today, but decades ahead.
-
If you’ve been told “you’ve got a slipped vertebra” and your plan so far has been uncertainty, waiting and fear — you might be ready for a proactive change.
Schedule your New Patient Experience and let us assess your spine, posture and alignment. Then we’ll map a clear plan together.
FAQs: Quick Answers You’ll Want
Q: Does a “slipped vertebra” mean my spine is broken?
A: No. The term usually refers to a small shift in alignment — not a fracture or collapse. Many cases are stable and manageable.
Q: If I have pain, does that mean I need surgery?
A: Not necessarily. Pain may come from nerve irritation or muscular compensation. If your slip is mild-to-moderate (grades 1-2) and you have no major nerve deficits, conservative care is often effective.
Q: Can posture correction really help reduce the amount of slip?
A: Yes — with the right structural corrective care, measurable improvements in alignment have been documented in research and in clinical practice.
Q: How long will it take before I feel better?
A: Every case is different. Some patients notice reduced symptoms early; alignment changes take time (weeks to months) and require consistency. Full correction may take longer, but you’ll progress step by step.
Q: What if I’ve already been told I’m not a candidate for non-surgical care?
A: It may be worth a second opinion. An advanced structural corrective approach (such as CBP) offers new options that weren’t always available in traditional models.
Bottom Line
Being told you have a “slipped vertebra” can be scary — but it doesn’t mean your spine is doomed. What really matters is:
-
How far the vertebra has shifted (the grade)
-
Whether the segment is unstable
-
Whether you are experiencing nerve pressure or major symptoms
-
Whether you’re being assessed properly (standing X-rays, posture analysis)
-
Whether you’re receiving structural corrective care (not just symptom management)
At 100+Living Health Centres, that’s exactly what we focus on. We believe in real, measurable structural improvement. We believe you can get relief, restore posture, and protect your spine for the long-term.
If you’re ready to take control of your spine’s alignment and movement, schedule your New Patient Experience today. Let’s begin your journey to better posture, fewer symptoms, and stronger movement for life.