Have You Ever Noticed That After Your Yoga Class Your Back Pain Gets Worse?
You are trying to do everything right. You eat well, you stay active, and you go to yoga class to stretch out your stiff muscles and relax. Everyone tells you that yoga is the “gold standard” for back health.
So why do you feel worse the next day?
It is a frustrating and confusing experience. You might feel a sharp twinge during a pose, or maybe a dull, aching throb that wakes you up the next morning. You might even feel shooting pain down your leg (sciatica) that wasn’t there before.
If this sounds like you, you are not crazy, and you are not alone.
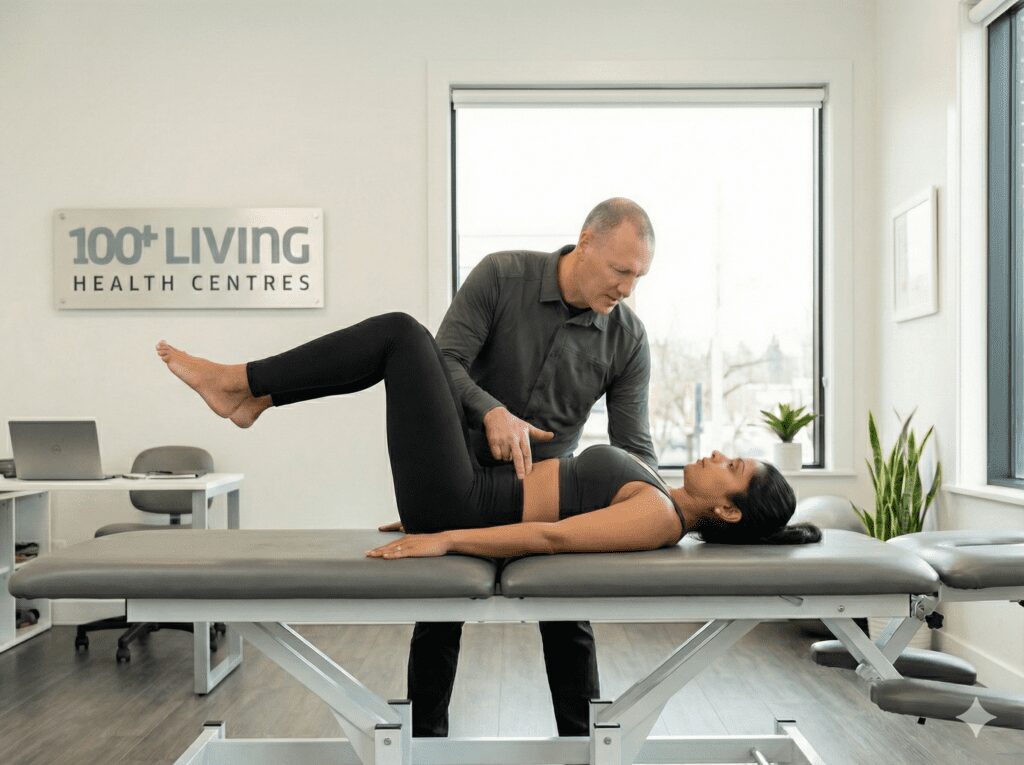
At 100+Living Health Centres here in Kelowna, I see this story play out almost every week. A patient comes in looking for relief because they tried to “stretch away” their back pain with yoga, but the pain only got louder.
The truth is, while yoga can be wonderful for many people, it is not a cure-all. In fact, if you have specific spinal conditions—some of which you might not even know about—certain yoga poses can actually trigger more pain and damage.
In this post, we are going to look at the science of why this happens. We will explore the hidden biomechanics of your spine, the specific conditions that hate yoga, and the research that explains why “doing it yourself” isn’t always the safest path.
The “Yoga Paradox”: Good Intentions, Bad Mechanics
Imagine you have a car with the front wheels out of alignment. If you drive that car slowly around a parking lot, you might not notice a problem. But if you take that car out on the highway and drive 100 km/h, the tires will wear out unevenly, the steering wheel will shake, and you might even cause an accident.
Driving the car wasn’t “bad.” Speed wasn’t “bad.” The problem was that you put stress (speed) on a structure that was misaligned.
Your spine works the same way.
Yoga is a form of mechanical stress. It asks your joints to move through a wide range of motion. If your spine is aligned and healthy, that movement is good. It feeds the joints and stretches the muscles.
But if your spine has a structural shift—like a twist, a loss of curve, or a slide—yoga acts like that highway drive. It puts force into a system that cannot handle it.
Research shows that yoga cannot correct the position of your spine.
According to research from Chiropractic BioPhysics (CBP) Non-Profit, yoga exercises can move joints through their existing range of motion, but they cannot correct a misaligned spine. If a bone is stuck or shifted out of place, yoga simply stretches the muscles around it, but it often forces the healthy joints above and below the problem area to move too much. This creates a new problem called instability.
Condition #1: The Spondylolisthesis Trap
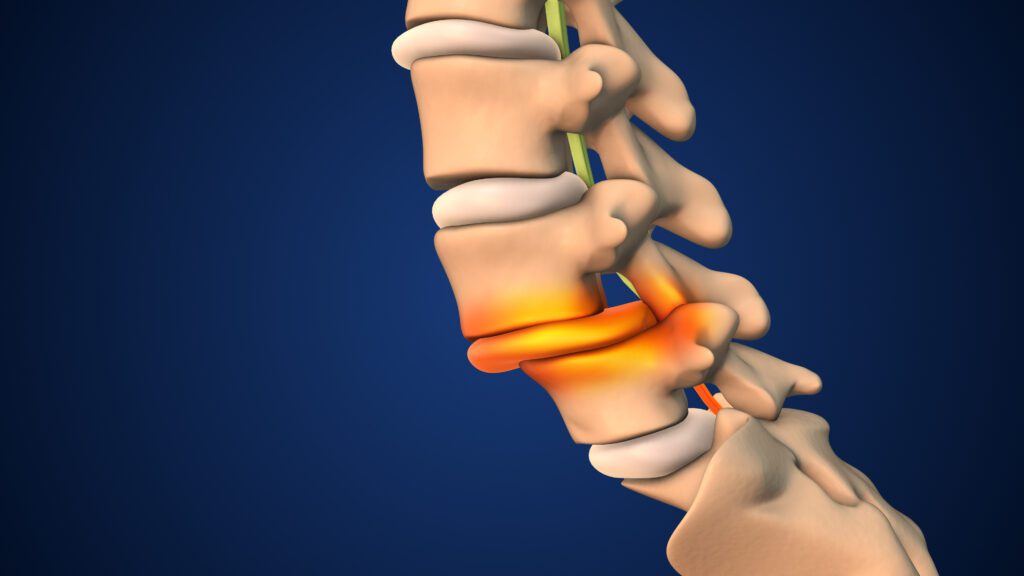
This is a big word, but it is a very common condition. Spondylolisthesis (spon-dee-lo-lis-thee-sis) happens when one of your vertebrae (usually in the lower back) slips forward over the bone below it.
This instability creates a lot of stress on the disc and the nerves. If you have this condition, your lower back is already unstable.
Why Yoga Can Make It Worse:
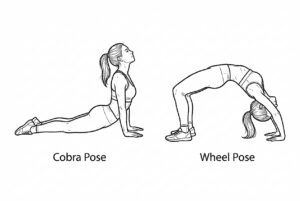
Many common yoga poses involve extension. This means bending backwards. Think of poses like:
-

Illustration of Cobra Pose and Wheel Pose Cobra
-
Upward-Facing Dog
-
Camel Pose
When you do these “back-bending” poses, you are physically pushing that slipped vertebra further forward. You are taking a bone that is already slipping and pushing it in the wrong direction.
This jams the joints together and can pinch the nerves tightly. This is often why you might feel okay during the class (because your muscles are warm), but the next day, you can barely stand up straight.
What the Science Says:
Research indicates that for patients with spondylolisthesis or “spondylolysis” (a stress fracture), hyperextension activities—like gymnastics or back-bending yoga poses—are a primary cause of pain and further slippage. The force of gravity combined with the backward bend creates a “shear force” that the damaged spine cannot handle.
Condition #2: The Hidden Scoliosis
Scoliosis is when the spine curves sideways. Many adults have mild scoliosis and don’t even know it. They just think one shoulder is lower than the other, or one pant leg always feels longer.
Scoliosis is not just a side-bend; it is also a twist. The spine twists like a corkscrew.
Why Yoga Can Make It Worse:
In a general yoga class, the instructor might tell the whole room to “twist to the right” to wring out the spine.
If you have scoliosis, your spine is already twisted.
-
If you twist in one direction, you might be relieving tension.
-
But if you twist in the other direction, you are twisting into the curve. This can lock up the joints and increase the rib hump (the bulge on one side of your back).
Furthermore, research from scoliosis experts warns that “Scoliosis Yoga” is not one-size-fits-all. Poses that bend the spine backwards can destabilize the thoracic spine (upper back) in scoliosis patients, making the curve progress faster.
Without an X-ray, you cannot know which way your spine is twisting. You are essentially flipping a coin with your spinal health every time you do a deep twist.
(For more on this, you can read my previous blog post on “Exercises to Avoid If You Have Scoliosis” or check the 100+ Living YouTube channel for safe alternatives.)
Condition #3: Sciatica and Disc Injuries
Sciatica is that sharp, electric-shock pain that travels down your leg. It is usually caused by a bulging disc pressing on the sciatic nerve.
Discs are like jelly donuts between your vertebrae. If you squeeze the front of the donut, the jelly shoots out the back.
Why Yoga Can Make It Worse:
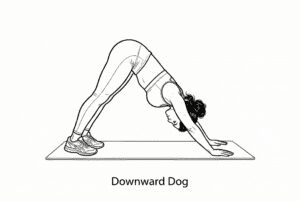
Many yoga classes involve a lot of forward folding.
-
Touching your toes
-
Seated forward fold
-

Illustration demonstrating Downward Dog Downward Dog
When you round your back forward, you are squeezing the front of the “donut.” This pushes the disc material backward—right into the nerve.
If you already have a posterior (backward) disc bulge, doing repeated forward folds is the exact mechanic that makes the injury worse. You might feel a stretch in your hamstrings, which feels “good” in the moment, but you are irritating the nerve root at the spine level.
Heidi Haavik’s Research: The Brain-Body Connection
Dr. Heidi Haavik is a neurophysiologist who studies how the spine affects the brain. Her research shows that when the spine is not moving correctly (subluxation), it changes the way your brain perceives your body. This is called altered sensorimotor integration.
Basically, your brain gets a “fuzzy” map of where your back is in space.
When you try to do complex yoga balance poses (like Tree Pose or Warrior III) with a “fuzzy map,” your brain cannot stabilize the muscles correctly. You might wobble, over-correct, or strain a muscle because your brain isn’t firing the right muscles at the right time.
You need a clear signal before you can demand complex movement from your body.
The “One-Size-Fits-All” Danger
The biggest problem isn’t yoga itself. The problem is the “group class” setting.
In a class of 20 people, the instructor creates a flow designed for the “average” healthy person. They do not have your X-rays. They do not know about your L5 spondylolisthesis or your T7 scoliosis.
They will cue you to “push deeper” or “find your edge.”
For a healthy spine, pushing to the edge is exercise.
For an injured or misaligned spine, pushing to the edge is trauma.
Biomechanics Are Unique
The biomechanics of the human spine are as unique as a fingerprint.
-
Some people have hyper-mobility (loose joints). They should never stretch deeply because their ligaments are already too loose. They need stability, not flexibility.
-
Some people have hypo-mobility (stiff joints). They need mobilization, but only in specific directions.
Research published by the Journal of Manipulative and Physiological Therapeutics has shown that specific traction (like the methods we use in CBP) is effective because it is distinct from general exercise. It targets the structure, whereas general exercise just targets the muscles.
If you treat a structural problem with a muscular solution (yoga), you will often fail to get long-term relief.
So, Should You Quit Yoga?
Not necessarily. But you need to change the order of operations.
Step 1: Analysis
You cannot fix what you cannot see. Before you start a new exercise routine—especially one that involves twisting and bending your spine—you need to know what your spine looks like.
This is where Advanced Certified Chiropractic BioPhysics (CBP) comes in.
Unlike general chiropractic which focuses on symptom relief, CBP is focused on structural correction.
At 100+Living, we use digital X-rays and posture analysis software to measure your spine down to the millimeter. We look for:
-
Spondylolisthesis (slippage).
-
Scoliosis (curves and twists).
-
Hypolordosis (loss of good curve).
-
Disc damage.
Step 2: Diagnosis & Guidance
Once we have your “blueprints,” we can tell you exactly what your body can tolerate.
-
If you have a slip, we will tell you: “No back bends.”
-
If you have a disc bulge, we will tell you: “No forward folds.”
-
If you have scoliosis, we will give you “Mirror Image” exercises that are unique to your curve, rather than generic twists.
Step 3: Corrective Care
We use Mirror Image Adjustments, 3-D Traction, and the Denneroll system to actually change the shape of the spine. We don’t just stretch it; we remodel it.
Step 4: Return to Activity
Once your spine is stable and the “brain-body” connection is clear (thanks to the adjustments improving that sensorimotor integration Dr. Haavik talks about), then you can return to yoga. And you will be able to do it safely, without the fear of waking up in pain.
What You Should Do Next
If you have noticed that yoga, Pilates, or even gym workouts are triggering your back pain or sciatica, stop guessing.
You are likely aggravating a hidden condition. Continuing to push through the pain could lead to more serious injury or the need for more invasive treatments later.
Start with a Free Consultation
I want to help you find the root cause. I invite you to book a Free 10-Minute Phone Consult with me. We can discuss your symptoms, your current exercise routine, and see if you are a candidate for a full Structural Analysis.
Or, if you are ready to get answers now, you can Schedule Your New Patient Experience at our Kelowna centre. This includes your exam, nerve scans, and the necessary X-rays to see exactly what is happening in your spine.
Take the Next Step
Don’t settle for temporary relief. Get care that helps correct the cause of your condition.
Step 1:
Start with a free 10-minute phone consult to discuss your symptoms and see if our approach is right for you.
Step 2:
Book your first comprehensive exam and consultation and get started.
Additional Resources
-
Watch on YouTube: Visit the 100+Living YouTube Channel for videos on “Exercises to Avoid for Spondylolisthesis” and safe core strengthening.
-
Read More: Check out my previous blog post on Exercises You Want to Avoid If You Have Scoliosis.
Remember: Your health is your greatest asset. Treat your spine with the respect it deserves. Don’t just move—move right.
About Dr. Graham Jenkins
Dr. Graham Jenkins is a chiropractor with over 30 years of experience and is the founder of 100+Living Health Centers in Kelowna, BC. He is the only Advanced Certified Chiropractic BioPhysics (CBP) doctor in the Interior of British Columbia.
Dr. Jenkins is passionate about longevity and helps families live long, strong, vibrant lives through posture restoration and neurological correction. He collaborates with researchers at Carleton University and UBC on spinal rehab and immune function.
Disclaimer: This content is for educational purposes only and does not replace professional medical advice. Always consult a qualified healthcare provider before making changes to your health plan.
References
-
Chiropractic BioPhysics Non-Profit. “Does practicing yoga eliminate the need for chiropractic care?” IdealSpine.com.
-
Haavik, H., et al. “The contemporary model of vertebral subluxation: A sensorimotor integration perspective.” Journal of the Council on Chiropractic Practice.
-
Hudson Valley Scoliosis. “Contraindicated Yoga Poses For Scoliosis: Moves To Avoid.”
-
Bene Yoga Therapy. “Yoga therapy for spondylolisthesis: Avoiding movements that aggravate pain.”
-
Pro Remedy Physio. “Avoid These Exercises if You Have Spondylolisthesis: In-Depth Guide.”
-
Moustafa, I.M., Diab, A.A. “Rehabilitation for Pain and Lumbar Segmental Motion in Chronic Mechanical Low Back Pain: A Randomized Trial.” Journal of Manipulative and Physiological Therapeutics.