The Great Debate: Should I Freeze It or Cook It?
It is the most common question I get in my clinic. A patient walks in, holding their lower back, looking exhausted and in pain. They sit down carefully and ask, “Doc, I have a slipped disc. Should I be putting ice on it, or should I be using a heating pad?”
If you go online, you will find a million different answers. Some websites say, “Ice for the first 48 hours only!” Others say, “Heat for muscle spasms!” It is enough to make your head spin—and your back hurt even more.
The truth is, both ice and heat are powerful tools. But like any tool, they only work if you use them at the right time for the right job.
If you use heat when your back is inflamed, you might make the swelling worse. If you use ice when your back is stiff and cold, you might lock up your muscles even tighter.
After 30+ years of treating patients with spinal issues, I have developed a simple clinical rule that helps clear up the confusion. I call it the “AM/PM Protocol.”
It goes like this: Heat in the morning. Ice in the afternoon.
In this post, we are going to dive deep into why this works. We will look at the science of your spine, the “circadian rhythm” of your discs, and how to use this simple strategy to finally get some relief and a good night’s sleep.
What Exactly Is a “Slipped Disc”?
Before we fix it, we have to understand what it is.
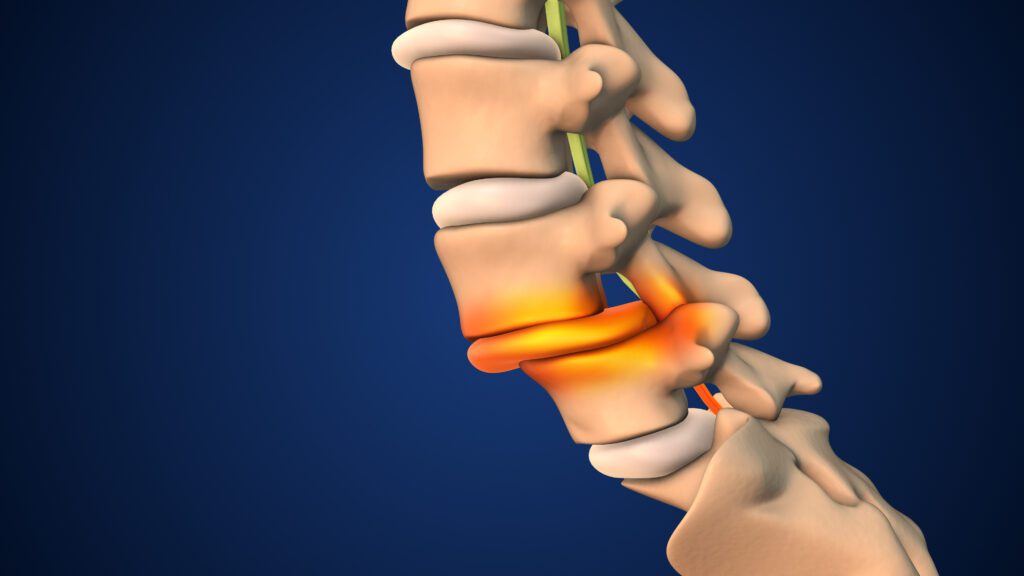
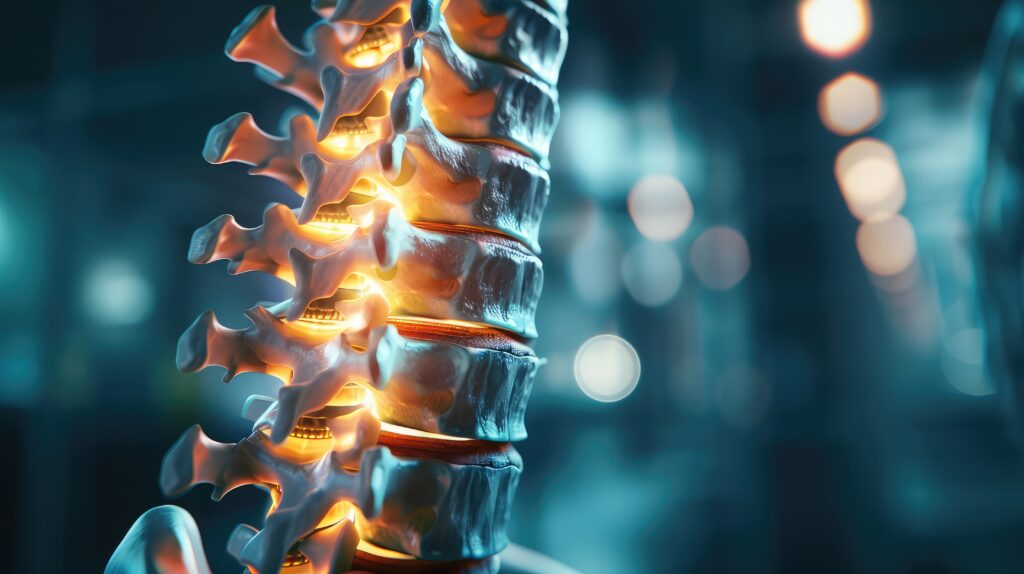
Your spine is made of 24 movable bones called vertebrae. Between each pair of bones, there is a soft, squishy cushion called a disc.
I like to think of the disc like a jelly donut.
-
The outside of the donut is tough and fibrous (called the annulus fibrosus).
-
The inside is filled with a soft jelly (called the nucleus pulposus).
A “slipped disc” (or herniated disc) happens when that tough outer layer tears or cracks. The jelly from the inside pushes out through the crack.
This jelly lands on the sensitive nerves that run down your back and into your legs. This is what causes that shooting pain, numbness, or that deep, dull ache that just won’t go away.
When this happens, your body reacts in two ways:
-
Stiffness: Your muscles tighten up to “guard” the injury.
-
Inflammation: Your body rushes blood and fluid to the area to try to heal it, causing swelling.
This is where the confusion comes in. You have stiffness (which needs heat) AND inflammation (which needs ice). So, how do you treat both without making the other one worse?
The Solution: Timing Is Everything
Your body is not the same at 7:00 AM as it is at 7:00 PM.
Your body runs on a 24-hour clock called a circadian rhythm. Your hormones, your body temperature, and even the height of your discs change throughout the day.
This means your back has different needs depending on what time it is.
Morning Goal: Mobilize and Move
When you wake up, your body has been still for 6 to 8 hours (hopefully). Your heart rate is low, your body temperature is lower, and your fluids have settled.
Research shows that for many joint and spinal conditions, stiffness is at its absolute peak in the morning. Your muscles are cold, and the “jelly” in your discs is thicker and more viscous.
If you try to move a cold, stiff engine, it might break. You need to warm it up first.
Afternoon Goal: Cool and Calm
By the time you get to the afternoon (around 2:00 PM or later), the story has changed. You have been walking, sitting, standing, and moving for hours.
Even if you have been careful, gravity has been pushing down on your spine all day. The cumulative stress of the day causes inflammation to build up. This is often why pain starts to throb or ache more towards the evening.
If you add heat now, you might throw fuel on the fire. You need to cool it down.
Part 1: Why We Use Heat in the Morning
Imagine trying to stretch a rubber band that has been in the freezer. It snaps, right? Now imagine stretching a rubber band that has been sitting in the sun. It stretches easily.
Your muscles and ligaments work the same way.
1. Increasing Blood Flow Heat causes your blood vessels to open up (dilate). This brings a rush of warm, oxygen-rich blood to the area. This fresh blood brings nutrients that your tissues need to wake up and start functioning.
2. Changing Tissue Elasticity Research shows that heat therapy improves the “elasticity” of soft tissues. This means your muscles and ligaments can stretch further without injury.
If you have a slipped disc, the muscles around it are often in a protective spasm. Heat helps these muscles relax, which takes the pressure off the disc and allows you to move more freely to start your day.
3. The “Gel” Effect While we don’t have a specific study on “heating spinal jelly,” we know from physics that fluids flow better when they are warm. Warming up your lower back helps the fluids in and around the spinal joints move more freely, reducing that “rusty hinge” feeling you have when you first get out of bed.
My Recommendation: As soon as you wake up, use moist heat. A hot shower is good, but a moist heating pad or a hot water bottle wrapped in a damp towel is even better. Apply it for 15 to 20 minutes.
This prepares your spine for the day. It tells your body, “It is safe to move.”
Part 2: Why We Use Ice After 2:00 PM
Now, let’s fast forward to the afternoon.
You have put in a half-day of work. Maybe you sat at a desk (which puts huge pressure on discs), or maybe you were on your feet.
Even if you don’t feel “sharp” pain yet, your body has been fighting gravity all day. The inflammation is starting to pool around that injured disc.
1. The Accumulation of Inflammation Inflammation is a chemical process. Throughout the day, as you irritate the tissue, your body releases chemicals called “cytokines” that cause swelling.
If you put heat on this now, you bring more blood and more fluid to an area that is already swollen. This can increase the pressure on the nerve.
2. Numbing the Pain Ice is a fantastic natural painkiller (analgesic). It works by slowing down the nerve signals. Basically, it makes the nerves “talk slower” so the pain signal doesn’t reach your brain as fast.
3. Preparing for Sleep This is the most critical part. Many patients with slipped discs can’t sleep because of the throbbing ache.
By using ice in the late afternoon or evening, you help “shut down” the inflammatory process before bed. You are physically cooling the tissues, constricting the blood vessels, and pushing the swelling out of the area.
Research from the Journal of Athletic Training confirms that ice is effective at reducing pain and swelling in musculoskeletal conditions. By doing this in the evening, you create a calmer environment in your spine, which can help you fall asleep easier.
My Recommendation: From 2:00 PM onwards, switch to ice. Use an ice pack (wrapped in a thin towel—never directly on skin!) for 15 to 20 minutes. You can do this when you get home from work, and again about an hour before bed.
The “CBP Difference”: Why Structure Matters
While ice and heat are great for managing symptoms, we have to ask the bigger question: Why did the disc slip in the first place?
Discs don’t usually just slip for no reason. Usually, it happens because the structure of the spine has shifted.
Think of your spine like the frame of a car. If the frame is bent, the tires (your discs) are going to wear out unevenly and eventually blow out.
You can put ice on the tire, and you can put heat on the tire, but if the frame is still bent, the tire will keep wearing out.
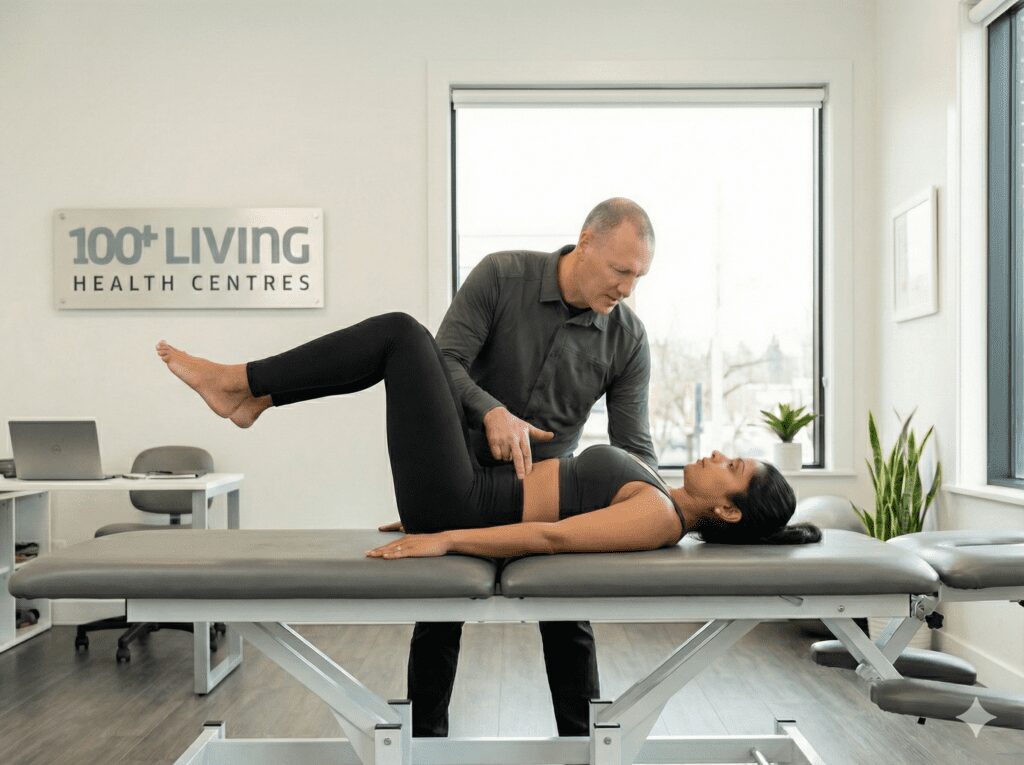
This is where Chiropractic BioPhysics (CBP) comes in.
We don’t just treat the pain (the symptom). We look for the structural shift (the cause). By correcting the alignment of the spine—restoring the natural curves—we take the uneven pressure off the disc. This allows the disc to actually heal, rather than just feeling better for a few hours.
Research shows that the mechanical characteristics of the disc are deeply tied to how they are loaded. If we fix the load, we fix the disc.
How We Measure Your Health: Beyond Just “Feeling Good”
At 100+ Living Health Centers, we don’t guess about your health. We measure it.
Most clinics might just poke your back or ask where it hurts. We need to know how your body is functioning on the inside. That is why we use four specific diagnostic tools to get a complete picture of your health:
1. Digital X-Rays (The Blueprint)
You cannot fix what you cannot see. Standard X-rays are often just looking for broken bones, but we use high-precision Digital X-Rays to measure the angles of your spine. Why it matters: We need to see the exact space between your vertebrae. If a space is too narrow, it tells us exactly which disc is degenerating or slipping. This is our roadmap for your care.
2. Digital Posture Analysis (The External View)
We use advanced software to scan your body’s alignment from the outside. Why it matters: We look for shifts in your center of gravity. Is your head forward? Is one hip higher than the other? These external shifts tell us where gravity is crushing your discs the hardest.
3. Heart Rate Variability (HRV) (The Neurological View)
You might have heard of HRV on smartwatches, but we use clinical-grade technology to measure it. What it measures: The balance between your “stress” system (Fight or Flight) and your “healing” system (Rest and Digest). Why it matters: Pain is stressful. A slipped disc puts your body in constant survival mode.
-
Low HRV: Means your body is stuck in stress. It is fighting so hard it cannot focus on healing the disc.
-
High HRV: Means your body is adaptable and ready to repair tissue. By tracking this, we can see if your nervous system is actually calming down as we correct your spine.
4. Spirometry (The Functional View)
This is a test that measures how well your lungs are working. What it measures: How much air you can breathe in and how fast you can blow it out. Why it matters: Oxygen is the fuel for healing. If your posture is poor—for example, if you have “Forward Head Posture” or a rounded upper back (hyperkyphosis)—your rib cage is physically compressed. You literally cannot take a full breath. Research shows that as posture worsens, lung capacity drops. If you aren’t getting full oxygen, your discs and tissues can’t heal as fast. We measure this to ensure your posture correction is actually improving your vitality and oxygen intake.
Red Flags: When to Call the Doctor Immediately
While most back pain can be managed, there are signs that you have a serious emergency. If you experience any of these, stop reading and go to the hospital or call a specialist immediately:
-
Loss of Bowel or Bladder Control: If you can’t go to the bathroom, or you can’t stop going, this is a medical emergency called Cauda Equina Syndrome.
-
Saddle Anesthesia: Numbness in your “saddle area” (inner thighs and groin).
-
Severe Foot Drop: If you try to walk and your foot just flops down, it means the nerve is severely compromised.
Your Action Plan: The AM/PM Protocol
So, here is your cheat sheet for the next time your back acts up:
-
Morning (Wake Up – Noon): HEAT.
-
Goal: Warm up the engine.
-
Method: Hot shower, moist heating pad.
-
Time: 15-20 minutes.
-
Result: Less stiffness, better mobility.
-
-
Afternoon (2:00 PM – Bedtime): ICE.
-
Goal: Cool down the inflammation.
-
Method: Gel pack, frozen peas (wrapped in a towel).
-
Time: 15-20 minutes.
-
Result: Less throbbing, better sleep.
-
-
All Day: Listen to your body.
-
If something hurts, stop doing it.
-
Ready to Fix the Frame?
Managing the pain with ice and heat is a great start. But if you are tired of living your life around your back pain, it is time to look at the structure.
At 100+ Living Health Centers, we specialize in finding the root cause of the problem. We don’t guess—we test.
We are the only Advanced Certified CBP office in the Interior of British Columbia. We use hospital-grade Digital X-Rays, Digital Posture Analysis, HRV stress testing, and Spirometry to see exactly what is happening to your body.
If you are in the Kelowna area, I invite you to stop guessing and start healing.
Take the Next Step
Don’t settle for temporary relief. Get care that helps correct the cause of your condition.
Step 1:
Start with a free 10-minute phone consult to discuss your symptoms and see if our approach is right for you.
Step 2:
Book your first comprehensive exam and consultation and get started.
Don’t let a slipped disc dictate your life. Use your heat, use your ice, and then come see us to fix it for good.
About Dr. Graham Jenkins
Dr. Graham Jenkins is a chiropractor with over 30 years of clinical experience. He is the founder of 100+ Living Health Centers in Kelowna, BC.
Dr. Jenkins is one of only two doctors in all of Western Canada to hold an Advanced Certification in Chiropractic BioPhysics (CBP). This advanced training allows him to perform structural rehabilitation of the spine, helping patients correct posture, reduce pain, and improve longevity.
He is passionate about evidence-based care and collaborates with researchers at Carleton University and UBC on spinal health and immune function. When he isn’t in the clinic, you can find him living the “100+ Lifestyle”—staying active, eating well, and enjoying the beautiful Okanagan outdoors.
Disclaimer: This content is for educational purposes only and does not replace professional medical advice. Always consult a qualified healthcare provider before making changes to your health plan.
References
-
Knaub, M. (2017). “When To Use Heat or Ice.” Penn State Spine Center. (Advice on using heat for muscle relaxation and blood flow).
-
Strathcona Physical Therapy. (2025). “Ice Application for Pain and Swelling: Evidence-Backed Effectiveness.” Journal of Athletic Training & British Journal of Sports Medicine. (Clinical trials supporting ice for reducing pain and swelling).
-
Tufts School of Medicine. (2024). “Are You Using Heat and Ice Properly?” (Explaining the anti-inflammatory mechanism of ice vs. the circulation boost of heat).
-
Healthline. (2019). “Heating Pads for Back Pain: Benefits and Best Practices.” (Benefits of heat for stiffness and circulation).
-
GoodRx. (2025). “Ice or Heat: Which Is Better for Treating Back Pain?” (Guidelines on using heat for mobility and ice for inflammation).
-
Frontiers in Cell and Developmental Biology. (2025). “Chronotherapy and intervertebral disc degeneration: understanding the role of circadian rhythm in degenerative processes.” (Evidence of circadian rhythms in disc height and stress).
-
Yoshida, K., et al. “Circadian rhythm and joint stiffness/destruction in rheumatoid arthritis.” Open Access Journals. (Identifying morning stiffness peaks).
-
The Rheumatologist. “Rheumatology with Rhythm.” (Cytokine cycles and inflammation timing).
-
Betterhood. (2025). “Using Heat and Support Together for Maximum Lower Back Relief.” (Heat for dilating blood vessels and relaxing spasms).
-
RACGP. (2021). “Heat therapy for low back pain.” (Guidelines for heat application times).
-
TADC Chiropractic Wellness Center. “The Efficacy of Cryotherapy in Treating Back Pain.” (Mechanisms of cryotherapy for nerve conduction and pain relief).
-
Riverside Sports Therapy. (2025). “How Cryotherapy Helps Manage Pain and Inflammation.” (Cellular effects of cold on inflammation pathways).
-
HealthLink BC. “Use Heat or Ice to Relieve Low Back Pain.” (Practical advice on timing ice application before bed).